|
Research Article
Vaginal prostaglandin E2 versus oxytocin for induction of labor in women with prelabor rupture of membranes at term
1 Registrar in Obstetrics & Gynaecology, Colombo North Teaching Hospital, Ragama, Sri Lanka
2 Professor in Obstetrics & Gynaecology, Colombo North Teaching Hospital, Ragama, Sri Lanka
Address correspondence to:
DPL Rasanjana
526/3, Heenkenda, Ragama,
Sri Lanka
Message to Corresponding Author
Article ID: 100011M01DR2022
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Rasanjana DPL, Wijesinghe PS, Gunarathna SMSG, Rathnayaka NMNB. Vaginal prostaglandin E2 versus oxytocin for induction of labor in women with prelabor rupture of membranes at term. Edorium J Matern Child Health 2022;7(2):1–7.ABSTRACT
Aims: Majority of women with prelabor rupture of membranes (PROM) at term will go in to labor within 24 hours. However early delivery will reduce the maternal and fetal infection and reduce the need for antibiotics for newborn. It will also increase maternal satisfaction. Oxytocin is being used for several decades for induction of labor in PROM. Prostaglandin E2 (PGE2) has shown promising results for the same purpose. A randomized controlled trial carried out to determine the effectiveness and acceptability of vaginal prostaglandin E2 for induction of labor in women with PROM at term.
Methods: A total of 162 women with singleton pregnancies at >37 weeks, cephalic presentations, Bishop scores of <6 were randomly allocated to receive either oxytocin or vaginal PGE2. The primary outcome measure was induction to delivery interval. Secondary outcomes were caesarean section rate, postpartum maternal fever, neonatal fever, and special care baby unit (SCBU) admissions.
Results: The induction to delivery interval was not significantly different (p -0.558) in oxytocin group (630.9 + 31.1 min) as compared to PGE2 group (635.2 + 27.1 min). Incidence of postpartum maternal fever, neonatal fever, and SCBU admission were almost similar in both groups. Uncomplicated vaginal delivery rates 2022were almost same in both groups (65.3% in PG group and 62.5% in oxytocin group).
Conclusion: Vaginal PGE2 appears to be as efficient as oxytocin for labor induction in term pregnancies with PROM and unfavorable cervices. However PGE2 doesn’t have additional advantages over oxytocin. As vaginal PGE2 is more expensive, it is rational to opt for oxytocin infusion to induce labor in term prelabor rupture of membranes accompanied with low Bishop’s scores.
Keywords: Induction, Oxytocin, Prelabor rupture of membranes instead of PROM, Prostaglandin E2
Introduction
Prelabor rupture of membranes (PROM) is a common clinical problem faced in everyday obstetric practice. In general PROM refers to rupture of membranes with leakage of amniotic fluids in the absence of uterine activity [1]. It occurs in approximately 8% of term pregnancies [2].
Prelabor rupture of membranes at term is commonly associated with over distention of uterus (e.g., multiple pregnancies or polyhydroamnios), cigarette smoking, coitus, frequent digital examination, altered mechanical properties of amniotic membrane, and infection [3],[4]. Prelabor rupture of membranes may result risk of immediate complications such as placental abruption, cord prolapse, and later complications such as maternal or neonatal infection, the necessity of interventions such as operative vaginal delivery and caesarean section [5],[6]. The diagnosis of spontaneous rupture of membranes is best achieved by maternal history followed by a sterile speculum examination [7]. Prelabor rupture of membranes at term may be managed expectantly or by elective birth with induction of labor. If labor is not induced, over 60% of these women will go into spontaneous labor within 24 hours and over 95% will go into labor spontaneously within 72 hours [8]. Induction of labor with oxytocin is the most commonly used intervention. However induction in the presence of an unfavorable cervix may lead to prolonged labor, failed induction and increased caesarean section rate. In contrast, continuation of pregnancy with expectant management may increase the risk of infections and also the maternal anxiety. Due to the conflicting conclusions regarding management of PROM, different obstetric units have different management protocols. Some prefer immediate induction and others wait for spontaneous onset of labor. If we can induce labor in a patient with favorable cervix we would be able to reduce the incidence of prolonged labor, failed inductions, and caesarean sections. Published literature conspicuously lacks any study conducted on the use of prostaglandin E2 in Sri Lanka. This study is therefore aimed at to determine the effectiveness and acceptability of vaginal prostaglandin E2 for induction of labor in women with PROM at term.
Expectant management of term PROM has been associated with chorioamnionitis and postpartum endometritis [9]. These infections may result in increased neonatal infection and mortality [10]. Some reports have projected that the risk of maternal and fetal infection increase proportionately with the time from membrane rupture to birth [11],[12] while others refute it [13]. However women were more satisfied with the care when the time gap between rupture of membranes and birth is short. Decision to induce labor may depend on the state of the cervix. Induction with insufficiently ripe cervix results in prolonged labor, increased requirement for analgesics and failed induction requiring caesarean section [14].
Published literature reveals conflicting conclusions on management of PROM at term [15],[16]. Hallak and colleagues reported that longer interval from rupture of membranes to birth is associated with increased incidence of caesarean section rates, maternal diarrhea, and neonatal intensive care admission [4]. A retrospective study has reported increased perinatal mortality and intrapartum fever in women when the delivery was delayed for more than 72 hours.
Mozurkewich and colleagues highlighted the benefits of induction of labor, with reduced rates of chorioamnionitis, endometritis, and neonatal infection. However caesarean section rate was significantly high [17]. The Canadian TERMPROM study [18] and subsequent secondary analysis provided considerable evidence regarding this issue. The trial compared four management policies, namely immediate induction with oxytocin, immediate induction with vaginal PGE2, expectant management (for maximum up to four days) followed by induction with oxytocin, or expectant management followed by induction with vaginal PGE2. Conclusion of this trial reveals, induction of labor in women with PROM (with oxytocin or prostaglandin E2) and expectant management result in similar rates of cesarean section and neonatal infection. Induction of labor with oxytocin results in a lesser incidence of maternal infection than with expectant management. Women view induction of labor more positively than expectant management.
A systematic review was performed by Dare and colleagues to compare outcomes following induction of labor (with oxytocin or prostaglandin E2) with expectant management. Twelve randomized controlled trials with a total of 6814 women were included in that review. Caesarean section and operative vaginal delivery rates were similar with either management approach. However incidence of chorioamnionitis is lesser with early induction as compared to expectant management. Fifty women should be induced to avoid single case of chorioamnionitis. Incidence of endometritis was also lower in the induction groups (RR 0.30; 95% CI, 0.12–0.74; four trials, 445 women). Time from rupture of membranes to delivery was significantly reduced with induction of labor. It was reduced by 13 hours in women receiving oxytocin and by 8 hours in those receiving prostaglandin compared with expectant management. Women who underwent induction of labor also had higher rates of satisfaction. One study reported a case of uterine rupture. It has occurred following induction with prostaglandin and none were reported in the expectant management groups. However this difference was not statistically significant (95% CI, 0.12–68.50). The incidence of neonatal intensive care unit (NICU) admissions was less in the induction group. Twenty women need to be induced following PROM to avoid one case of NICU admission. One NICU admission was avoided for every 20 women induced for PROM. One large study reported that neonates born following expectant management were more likely to spend more than 24 hours in the NICU. However, there were no statistically significant differences between the two groups regarding infant success of breast-feeding or incidences of cord prolapse and neonatal infection.
MATERIALS AND METHODS
Study design and setting
This is a randomized controlled trial which was conducted at the university obstetrics unit Colombo North Teaching Hospital, Sri Lanka.
Study population (eligibility criteria)
Women were eligible for entry into the study if they had ruptured membranes, were at or more than 37 weeks of period of amenorrhea and had a single fetus in cephalic presentation with unfavorable cervix (modified Bishops score of 6 or less). Women were excluded from the study if they were in active labor, had previous caesarean section, meconium staining of amniotic fluid or maternal fever was already present.
Randomization
Using computer generated random numbers women were allocated into the study and control groups by stratified (primip, multip) block randomization. Sequentially numbered and sealed opaque envelopes coded with the management group prepared by a colleague according to random allocation sequence were used. Investigator was blinded.
Treatment protocol
Rupture of membranes was confirmed by speculum examination by the investigator and cervical assessment was done at the same time. After obtaining informed written consent, all eligible women were recruited to the study. They were randomly allocated to study or control groups as mentioned above. The time at which membrane rupture had occurred was considered as the starting point of time line and all events were carried out in relation to that.
Study group
Six hours after rupture of membranes, prostaglandin E2 3 mg tablet was inserted to posterior vaginal fornix by a colleague and cardio-tocographic (CTG) assessment was done at 2 hours and 4 hours after prostaglandin E2 insertion. If the woman went in to labor she was admitted to labor ward and allowed to progress. If she didn’t go into labor after 6 hours of prostaglandin E2 insertion (12 hours after rupture of membranes) she was admitted to labor ward and oxytocin infusion was started.
Control group
Cardio-tocographic (CTG) assessment was done after admission. After 6 hours of membrane rupture, the women was admitted to labor ward and oxytocin infusion was started.
Oxytocin infusion in both groups was carried out using infusion pumps. Oxytocin (5 IU in 50 mL of normal saline) was started at a rate of 4 mU/min and increased by 4 mU/min every 20 minutes for primips and by 2 mU every 20 minutes for multips. Oxytocin dose was not increased further, if maximum of four contractions were occurred during 10 minutes for two consecutive 10-minute periods. The maximum allowable dose of oxytocin was 32 mU/min. Progress of labor was assessed by a medical officer and documented on partogram (Figure 1).
Data collection
Data was collected using an interviewer questioner and ward bed head ticket (BHT) records.
Outcome measures
Caesarean section rate
Percentage of caesarean sections out of the total number of inductions for each arm.
Postpartum maternal fever
Axillary temperature was measured four times a day. Temperature rise above 100.4 °F (38 °C) maintained over 24 hours during first 72 hours of delivery was considered as postpartum maternal fever.
SCBU admission
Admission and stay for more than 24 hours in SCBU.
Neonatal fever
Axillary temperature was measured four times a day. Temperature rise above 100.4 °F (38 C) maintained over 24 hours during first 72 hours was considered as neonatal fever.
Induction to delivery interval
Duration from prostaglandin insertion to delivery of the baby was considered as induction to delivery interval for study group. Duration from starting oxytocin to delivery of the baby was considered as induction to delivery interval for control group.
RESULTS
A total of 162 pregnant women were included into the study. Following randomization, 82 women were allocated to PGE2 arm and 80 were allocated to the oxytocin arm. There were no dropouts and none of the participants were discontinued after enrolment to the study.
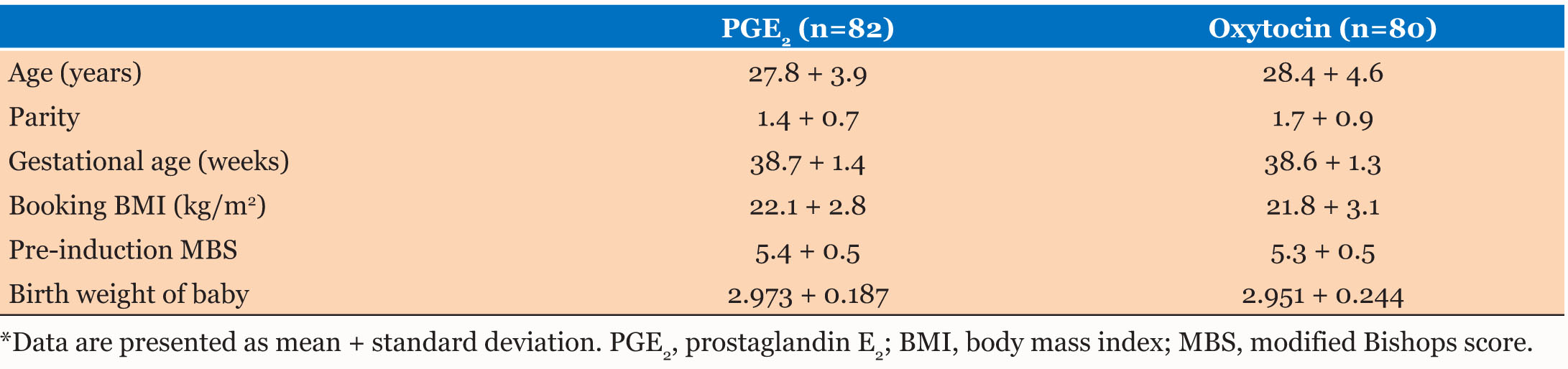
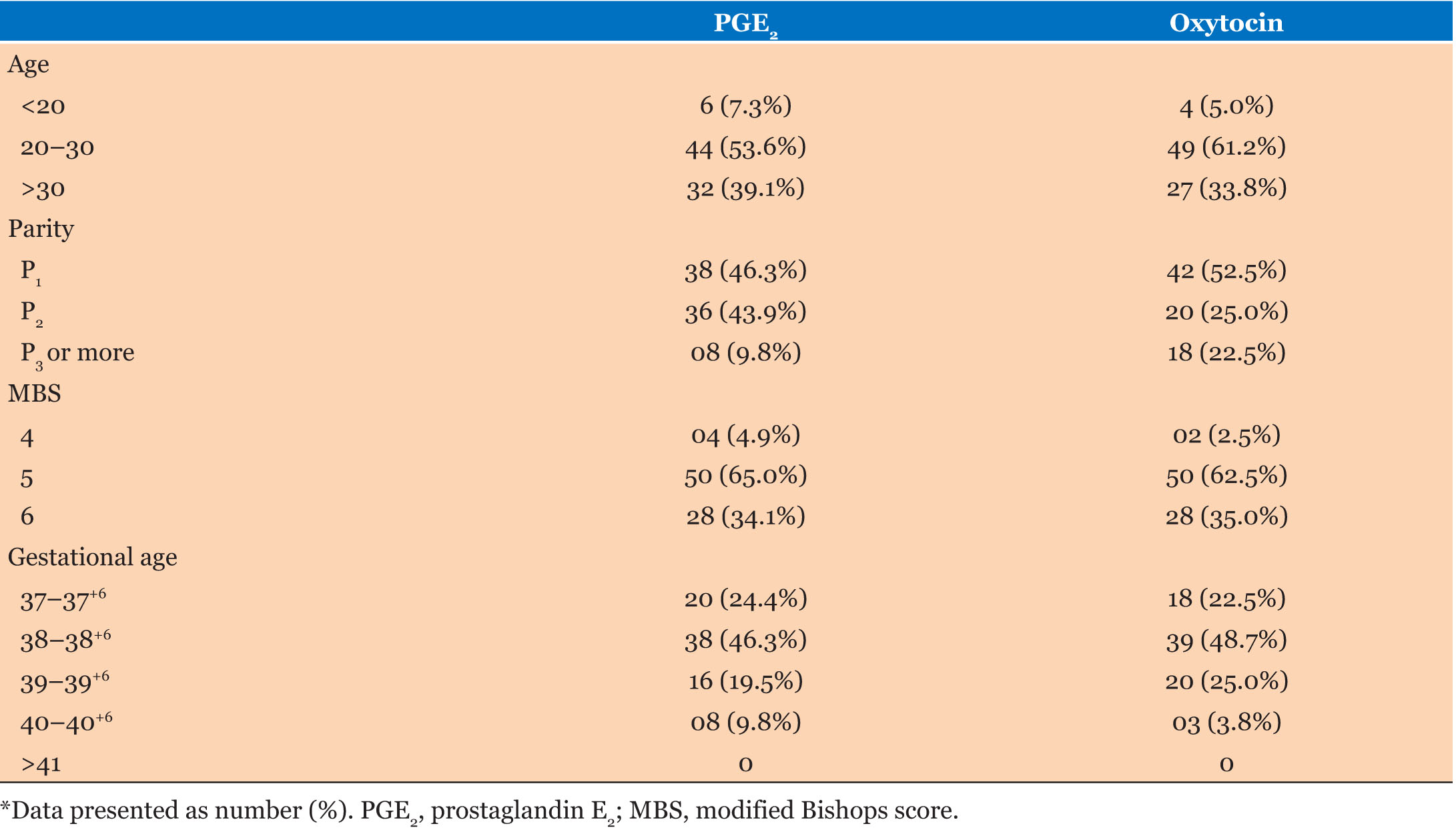
As observed from Table 1 and Table 2, there is no significant difference in control variables between two groups.
As observed from Table 3, induction to delivery interval was not significantly different (p -0.558) in oxytocin group (630.9 + 31.1 min) as compared to PGE2 group (635.2 + 27.1 min). Incidence of postpartum maternal fever, neonatal fever, and SCBU admission were almost similar in both groups. As observed from Table 4, uncomplicated vaginal delivery rates were almost same in both groups (65.3% in PG group and 62.5% in oxytocin group), whereas operative/assisted deliveries were more (9.7%) in PGE2 group than (2.5%) oxytocin group.
Discussion
Majority of women with prelabor rupture of membranes (PROM) at term will go into spontaneous labor within 24 hours. However early delivery will reduce the maternal and fetal infection and reduce the need for antibiotics for newborn. It will also increase maternal satisfaction.
The present study doesn’t show any statistically significant difference in time from induction to delivery between PGE2 and oxytocin groups. The study by Cigdem and colleagues [19] showed that oxytocin infusion significantly shortened the time from induction to delivery compared to vaginal PGE2 and they have concluded that vaginal PGE2 appears to be a relatively inefficient method of induction for PROM.
In the present study, the rates of uncomplicated vaginal deliveries were almost the same in PGE2 and oxytocin groups accounting 68.3% and 62.5% respectively. Operative vaginal deliveries were high in PGE2 group (9.7%) compared to oxytocin (2.5%). Though there is no statistically significant difference in caesarean section rates, in PGE2 group it is well below (21.9%) and in oxytocin group it is above (35.0%) the institution caesarean section rate for year 2014 (26.1%).
Some international studies have also failed to demonstrate any statistically significant difference with respect to the type of delivery after using prostaglandin compared to oxytocin [20],[21]. The lack of significant difference in caesarean delivery rates could easily be the result of type II error.
The commonest indication for caesarean section in PGE2 group was fetal distress (12) and among oxytocin group was poor progress of labor (14).
The other outcome measures in concern are those that reflect the condition at birth. They are also related to the process of labor induction and delivery, and the risk of infection in case of prelabor rupture of membrane. Apgar score at 1 minute, 5 minutes, and rate of SCBU admission are almost same in both study groups. These results are in the agreement with the current literature in which perinatal outcomes are normal even in cases of expectant management for long periods, provided care is taken to avoid digital vaginal examination and that there is no prior clinical evidence of chorioamnionitis [13],[21].
There is no significant difference between the two groups with regard to the postpartum maternal fever, though the incidence among PGE2 group is higher than the oxytocin group. Three out of four maternal fever cases in PGE2 group were associated with complications with caesarean section wound. However it should be remembered that the sample size estimate was not performed taking these factors into account and therefore the study does not have enough power to arrive at a definite conclusion in those aspects.
Conclusion
In conclusion, vaginal PGE2 appears to be as efficient as oxytocin for induction of labor in term pregnancies with prelabor rupture of membrane and unfavorable cervices. Prostaglandin E2 may initiate uterine contractions and maintain as effectively as oxytocin. However PGE2 doesn’t have additional advantages over oxytocin. As vaginal PGE2 is more expensive, it is rational to opt for oxytocin to induce labor in term prelabor rupture of membranes accompanied with low Bishop’s scores.
REFERENCES
1.
2.
Cammu H, Verlaenen H, Perde MP. Premature rupture of membranes at term in nulliparous women: A hazard? Obstet Gynecol 1990;76(4):671–4.
[Pubmed]

3.
Duff P. Premature rupture of the membranes in term patients. Semin Perinatol 1996;20(5):401–8. [CrossRef]
[Pubmed]

4.
5.
Alexander JM, Cox SM. Clinical course of premature rupture of the membranes. Semin Perinatol 1996;20(5):369–74. [CrossRef]
[Pubmed]

6.
Kong AS, Bates SJ, Rizk B. Rupture of membranes before the onset of spontaneous labour increases the likelihood of instrumental delivery. Br J Anaesth 1992;68(3):252–5. [CrossRef]
[Pubmed]

7.
8.
Conway DI, Prendiville WJ, Morris A, Speller DC, Stirrat GM. Management of spontaneous rupture of the membranes in the absence of labor in primigravid women at term. Am J Obstet Gynecol 1984;150(8):947–51. [CrossRef]
[Pubmed]

9.
Gonen R, Hannah ME, Milligan JE. Does prolonged preterm premature rupture of the membranes predispose to abruptio placentae? Obstet Gynecol 1989;74(3 Pt 1):347–50.
[Pubmed]

10.
Merenstein GB, Weisman LE. Premature rupture of the membranes: Neonatal consequences. Semin Perinatol 1996;20(5):375–80. [CrossRef]
[Pubmed]

11.
Gafni A, Goeree R, Myhr T, et al. Induction of labour versus expectant management for prelabour rupture of the membranes at term: An economic evaluation. TERMPROM Study Group. Term Prelabour Rupture of the Membranes. CMAJ 1997;157(11):1519–25.
[Pubmed]

12.
Zlatnik FJ. Management of premature rupture of membranes at term. Obstet Gynecol Clin North Am 1992;19(2):353–64.
[Pubmed]

13.
Seaward PG, Hannah ME, Myhr TL, et al. International Multicentre Term Prelabor Rupture of Membranes Study: Evaluation of predictors of clinical chorioamnionitis and postpartum fever in patients with prelabor rupture of membranes at term. Am J Obstet Gynecol 1997;177(5):1024–9. [CrossRef]
[Pubmed]

14.
Duff P. Premature rupture of the membranes in term patients: Induction of labor versus expectant management. Clin Obstet Gynecol 1998;41(4):883–91. [CrossRef]
[Pubmed]

15.
Crane JMG, Young DC. Induction of labour with a favourable cervix and/or pre-labour rupture of membranes. Best Pract Res Clin Obstet Gynaecol 2003;17(5):795–809. [CrossRef]
[Pubmed]

16.
Guise JM, Duff P, Christian JS. Management of term patients with premature rupture of membranes and an unfavorable cervix. Am J Perinatol 1992;9(1):56–60. [CrossRef]
[Pubmed]

17.
Mozurkewich EL, Wolf FM. Premature rupture of membranes at term: A meta-analysis of three management schemes. Obstet Gynecol 1997;89(6):1035–43. [CrossRef]
[Pubmed]

18.
Hannah ME, Ohlsson A, Farine D, et al. Induction of labour compared with expectant management for prelabour rupture of the membranes at term. TERMPROM study group. N Engl J Med 1996;334(16):1005–10. [CrossRef]
[Pubmed]

19.
Kunt C, Kanat-Pektas M, Gungor ANC, et al. Randomized trial of vaginal prostaglandin E2 versus oxytocin for labour induction in term premature rupture of membranes. Taiwan J Obstet Gynecol 2010;49(1):57–61. [CrossRef]
[Pubmed]

20.
Sanchez-Ramos L, Chen AH, Kaunitz AM, Gaudier FL, Delke I. Labour induction with intravaginal misoprostol in term premature rupture of membranes. A randomized study. Obstet Gynecol 1997;89(6):909–12. [CrossRef]
[Pubmed]

21.
Ozden S, Delikara MN, Aveci A, Fiçicioglu C. Intravaginal misoprostol vs. expectant management in premature rupture of membranes with low bishops scores at term. Int J Gynaecol Obstet 2002;77(2):109–15. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Acknowledgments
We would like to thank all the patients who participated in this clinical trial and to all the people who supported us throughout the study.
Author ContributionsDPL Rasanjana - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
PS Wijesinghe - Conception of the work, Design of the work, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
SMSG Gunarathna - Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
NMNB Rathnayaka - Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2022 DPL Rasanjana et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.