|
Research Article
The comparison of effectiveness of keeping transcervical foley catheter in situ for 12 hours versus 24 hours for cervical ripening: A randomized trial on nulliparous women with prolonged pregnancy
1 Registrar in Obstetrics and Gynaecology, Colombo North Teaching Hospital, Ragama, Sri Lanka
2 Consultant Obstetrician and Gynaecologist, Colombo North Teaching Hospital, Ragama, Sri Lanka
Address correspondence to:
Dilan Malinda Casather
11 Stone Yard Close, Ormskirk, Lancashire L39 AF,
United Kingdom
Message to Corresponding Author
Article ID: 100009M01DC2021
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Casather DM, Rajapaksha RNG. The comparison of effectiveness of keeping transcervical foley catheter in situ for 12 hours versus 24 hours for cervical ripening: A randomized trial on nulliparous women with prolonged pregnancy. Edorium J Matern Child Health 2021;6:100009M01DC2021.ABSTRACT
Aims: Post-term pregnancy has been associated with increased perinatal mortality and morbidity. Induction of labor is most challenging in nulliparous women with prolonged pregnancy. Although many methods are used to ripen the cervix before induction is attempted, there are little consensus on the best method. Our study compared the efficacy, acceptability, and safety of keeping transcervical catheter in situ for 12 hours versus 24 hours, for cervical ripening in healthy nulliparous women with an unfavorable cervix.
Methods: A non-blind randomized controlled trial was conducted in two groups of healthy primigravida with singleton pregnancy. Selected females were randomized into two treatment groups. Foley catheter was introduced to the space between the amniotic membrane and the lower segment of the uterus. Bishop’s scores were assessed after completion of 12 hours and 24 hours in the respective groups. The possible maternal and fetal adverse reactions of the procedure were assessed.
Results: There was no statistically significant difference in Bishop’s score, duration of labor and caesarean section rate in two groups. The Apgar score at 5 minutes, rate of special care baby unit admission, and neonatal sepsis were comparable in both groups. There were significantly more culture positive urinary tract infections seen in 2021women in the 24 hour group compared to the 12 hour group.
Conclusion: According to our study there were no major differences in effectiveness, acceptability and maternal and fetal side effects in compared groups. Culture positive urinary tract infections were slightly increased among the women in the 24 hour induction group.
Keywords: Cervical ripening, Foley catheter, Primigravida, Prolonged pregnancy
Introduction
The mean duration of a human pregnancy is 280 days from the first day of the last menstrual period. Post-term pregnancy is defined as gestation that has progressed beyond 294 completed days [1]. Post-term pregnancy is associated with increased perinatal mortality and morbidity as well as maternal morbidity [2],[3]. Fetal macrosomia, intrapartum fetal distress, meconium aspiration syndrome, shoulder dystocia, and post-maturity syndrome are the main causes for perinatal morbidity in prolong pregnancy. The perinatal morbidity in post-term pregnancy is primarily due to the placental insufficiency towards term [3],[4].
The obstetric complications associated with post-term pregnancy are mainly due to an unfavorable cervix at the time induction. This leads to prolonged labor, post-partum hemorrhage and traumatic vaginal birth due to instrumental delivery. These poor maternal and fetal outcomes may increase antenatal testing between 40 weeks and 42 weeks of gestation, and labor inductions with cervical ripening before 42 weeks of gestation [5]. Induction of labor is defined as the use of artificial methods to commence labor before spontaneous onset of labor. When the benefits of induction outweigh the risk to continue with a pregnancy, the induction of labor is considered. Even though, labor induction is one of the commonest procedures in obstetrics, occurring in up to 30–35% of pregnancies, over 40% of all cases result in induction failure due to the induction of an unfavorable cervix at the time of induction [6]. The success of labor induction depends mainly on cervical favorability before commencement of the induction. With the most favorable outcomes occurring in cervices which are soft, effaced, and modified Bishop’s score of more than 6 [7].
Although there are several methods used for pre-induction and ripening of the cervix, there is little evidence on the best method to be used in nulliparous women with prolonged pregnancy. The optimal method for cervical ripening in these women has not being described specifically [8]. Pharmacological and mechanical agents are use as cervical ripening methods. Prostaglandin E2 imitates normal cervical ripening and it enhances the oxytocin action on myometrium by increasing the oxytocin receptor sensitivity on myometrium. As it increases the likelihood of vaginal delivery to within 24–48 hours, vaginal prostaglandins have become the most commonly used pre-induction method in most industrialized countries. In addition to the membrane sweeping, the intracervical foley catheter is inserted in order to achieve cervical ripening. It has the capacity to modify the cervical status, by possible release of prostaglandins, but has limited effect on uterine contraction [9]. The WHO guideline recommends the intracervical foley catheter as one of the first-line methods of labor induction, and the number of foley catheter inductions is increasing worldwide, especially in poor economic countries [1]. Prostaglandin E2, vaginal pessaries, or vaginal gels are more expensive than foley catheters as pre-induction procedures. Additionally, foley catheter induction has more favorable secondary outcomes compared with prostaglandin E2 induction, in terms of fewer cases of uterine hyperstimulation, intrapartum fetal asphyxia, and neonatal intensive care admissions [10]. Hence, the popularity of intracervical foley catheter procedure is mainly due to cost effectiveness and relative reduction of frequency of adverse effects compared to the pharmacologic ripening methods such as prostaglandins [11].
Recent studies show that failed inductions still occur following foley catheter balloon ripening [12]. This prompted further studies, which evaluated the effectiveness of foley catheter induction with various modifications, such as, using double balloon catheters instead of single balloon catheters, by increasing the volume of the foley catheter bulb and the use of a transcervical foley catheter with extra-amniotic saline infusion [13],[14],[15]. Although, it is recommended to keep the foley catheter in situ for 12 to 24 hours [16]; no study has compared the effectiveness and safety of the procedure for these two time periods. This randomized controlled trial compared the efficacy, patient satisfaction, and safety of keeping transcervical foley catheter for 12 hours versus 24 hours for cervical ripening in nulliparous women with prolonged pregnancy.
MATERIALS AND METHODS
A randomized controlled trial was carried out including two groups of healthy primigravida with singleton pregnancy. The study was carried out at Colombo North Teaching Hospital Ragama, Sri Lanka, between August 2019 and April 2020. Twenty to thirty five years old nulliparous women with reliable pregnancy dating that includes a first trimester ultrasound scan between 10 weeks and 6 days and 13 weeks and 6 days were recruited to the study when they attended the antenatal clinic following 36 weeks of gestation. They were given an appointment for labor induction at 40 weeks and 3 days of gestation, as is the standard practice in our unit. Forty-six women declined to participate to the study.
Participants, who consented for the study, were admitted to the antenatal ward at 40 weeks and 3 days of gestation. Inclusion criteria for the study were singleton pregnancy, intact membranes, cephalic presentation and a reassuring fetal cardiac status by cardiotocography. Exclusion criteria were presence of painful uterine contractions (>1 in 30 minutes), antepartum hemorrhage, known gross fetal anomalies, and placenta previa. The presence of other contraindications to vaginal delivery was also considered as exclusion criteria. Two hundred sixty women did not meet the inclusion criteria and excluded from the study.
All women who met the eligible criteria were examined at 40 weeks and 3 days of gestation to assess the cervical status. Those who had a cervix which can permit the tip of the foley catheter and modified Bishop’s score [17] less than 5 were invited to participate in the investigation. The selected females were randomized into two treatment groups, using simple block randomization, with a computer generated randomization list with random number generator option in SAS statistical package (SAS Inc. version 15.1 for windows). Randomly selected participants were assigned to either the 12 hours foley catheter group or 24 hours foley catheter group according to the number generated by the software.
Bishop’s scores of the participants were assessed and the characteristics of the cervix (dilatation 0–3 points, effacement 0–3 points, station 0–3 points, consistency 0–2 points, and position 0–2 points) was recorded before the intervention. Participants were positioned in dorsal lithotomy position and Cusco’s bivalve self-retaining speculum was introduced to allow adequate visualization of the external cervical os of the cervix. Moreover, the cervix cleansed with 10% povidine iodine solution.
The interviewer introduced No 18, 30 mL foley catheter tip into the space between the amniotic membrane and the lower segment of the uterus with an artery forceps under direct vision with satisfactory lighting. Catheter bulb was inflated up to 30 mL with distilled water. The foley catheter taped with minor traction to the participant medial aspect of the thigh. Fetal monitoring by cardiotocography performed after inserting the catheter. The procedure abandoned and foley catheter was removed in cases of spontaneous rupture of the membranes, significant vaginal bleeding, major discomfort or pain, and two unsuccessful trials to introduce foley catheter into the cervical canal.
Routine antenatal care was given to both groups. Bishop’s scores were assessed after completion of 12 hours and 24 hours in the respective groups. Participants were sent to the labor room for induction of labor. Oxytocin infusion was commenced two hours following rupture of the amniotic membrane. Labor was managed by the intern medical officers, senior house officers, registrars, midwifes, nurses, and by obstetrician. Assessment of the labor was conducted with the partogram and the existing protocols of the unit.
Oxytocin infusion adjusted as required to maintain three to five regular moderate to strong contractions per 10 minutes duration. Continuous cardiotocography used throughout the established labor, and any cardiotocographic abnormality was recorded. In addition, color of the amniotic fluid documented in each vaginal examination.
Occurrence of five of more contractions in 10 minutes for two consecutive 10 minutes period or a contraction lasting at least 2 minutes considered as uterine hyperstimulation. Persistently reduced baseline variability, atypical variable decelerations, or late decelerations considered non-reassuring cardiotocography. Since there was no standard definition for failed induction of labor, cervical dilatation less than 5 cm after 8 hours of strong contraction was taken as failed induction. The possible adverse reactions of the procedure were assessed during cervical ripening, in labor and in puerperium including, vaginal bleeding, severity of the pain, uterine hyperstimulation, maternal, and neonatal infections. Twelve hours after and 24 hours after the foley insertion in 12 hour group and 24 hour groups the degree of discomfort was assed using Wong-Baker FACES Pain Rating Scale [18].
The sample size calculation was performed considering the primary outcome of the study. In this study Bishop’s scores at the time of induction were considered as primary outcome [19]. It has been done according to calculation criterion described elsewhere keeping 10% drop rate as well. The level of significance and power of test were set as 0.05% (p<0.05) and 0.8 (80%), respectively. To achieve this power, the study needed a sample size of 109 for each arm.
Interviewer estimated the Bishop’s scores at 12 hours and 24 hours after insertion of transcervical foley catheter in both groups separately. In addition to that, induction to delivery time, spontaneous catheter expulsion rate, duration of the labor, vaginal delivery rate, cesarean section rate, failed induction rate, number of vaginal examination during the labor, severity of pain and bleeding during cervical ripening, meconium stained liquor, cardiotocography abnormality during labor, maternal pyrexia during labor, and maternal and neonatal pyrexia rate during immediate (within three days) post-partum period, admission to the special care baby unit and antibiotic usage has been evaluated and documented in the data extraction sheet.
Both parametric and non-parametric data analysis techniques were employed depending on the distribution of data sets. Categorical data combined to obtain absolute and relative frequencies and percentages. While continuous data presented as means and standard deviations (SD). Chi-squared test was used to analyze the frequencies of the nominal variables in the cross tables where data distribution is normal, whereas Fisher’s exact test was used as the non-parametric test. Continuous data has been analyzed with the student t-test. In all cases, a p value of <0.05 was considered as statistically significant and the analysis was performed using the Statistical Package for Social Sciences (SPSS, USA) computer programme. Postgraduate Institute of Medicine in Sri Lanka approved the study and the ethical review committee of the Faculty of Medicine University of Kelaniya in Sri Lanka approved this study without alterations.
RESULTS
Recruitment
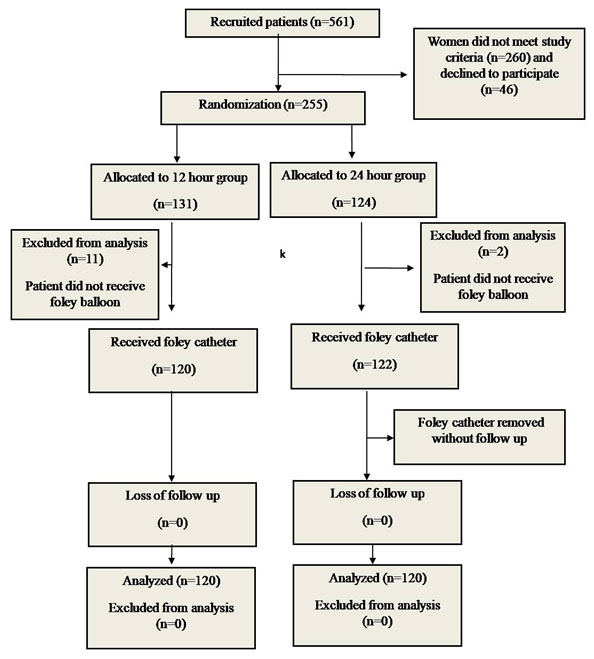
During the study period, 561 women were interviewed and 301 women had inclusion criteria. Forty six women declined to participate. Of the 255 women recruited, 13 women discontinued their induction during catheter insertion due to failed insertion. Of these 13 women, 11 of them were in the 12 hour induction group and 2 of them were in the 24 hour induction group. A total of 120 women received foley catheter in the 12 hour group and 122 women received foley catheter in the 24 hour induction group. Out of 122 women in 24 hour induction group 2 women demanded removal of catheter soon after the insertion due to the pain and discomfort. Thus, in each group 120 women completed the follow-up (Figure 1) and data available for the statistical analysis for the observed outcomes.
Demographical data
Both groups had similar baseline demographical parameters. Mean age of the participants in the 12 hour induction group was 28.01 years (±4.31), and mean age of the participants in the 24 induction hour group was 28.41 years (±4.57), (p =0.68).
Pre-induction results
Both groups had similar pre-induction Bishop’s scores. In the 12 hour induction group pre-induction Bishop’s score was 3.11 (±1.10) and in the 24 hour induction group pre-induction Bishop’s score was 3.23 (±1.11); (p=0.2).
Post-induction results
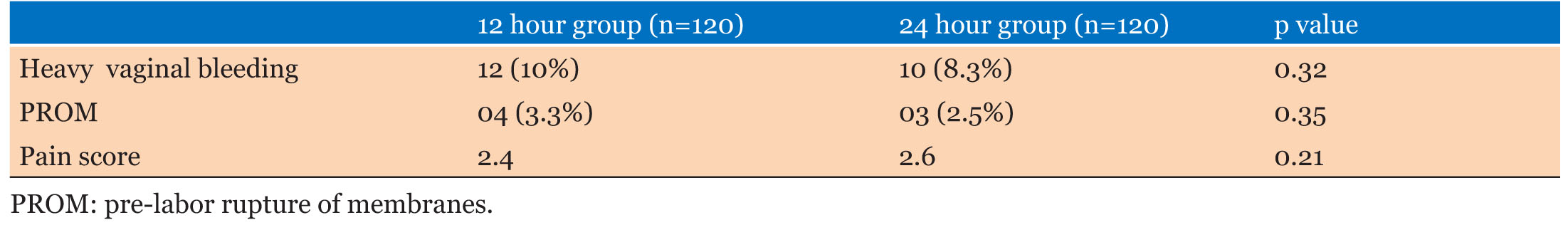
After foley catheter insertion 26 (21.6%) and 32 (26.6%) women had spontaneous expulsion of the catheter in 12 hour induction group and 24 hour induction group respectively. Following foley induction 12 (10%) women of the 12 hour group and 10 (8.3%) women of 24 hour induction group had heavy vaginal bleeding, whereas, pre-labor rupture of membrane was observed in only 4 (3.3%), and 3 (2.5%) women in the 12 hour group and the 24 hour group, respectively. Two women in the 12 hour induction group had non-reassuring fetal heart rate status following catheter insertion. Pain and discomfort were assessed and scored according to the Wong-Baker FACES Pain Rating Scale after 12 hours and after 24 hours in the respective groups, there was no difference in both groups. In the 12 hour group pain score was 2.4 and in the 24 hour group it was 2.6 (p=0.21) (Table 1).
Outcomes
Considering the primary outcome of the study, there was no statistically significant difference in Bishop’s score after 12 hours and 24 hour in both groups. In the 12 hour induction group post-induction Bishop’s score 7.2 and it was 7.4 in the 24 hour induction group (p=0.24), duration of the labor was also comparable in both groups (12 hour group: 455.1 minutes (±28.87) and 24 hour group 448.7 (±39.6); (p=0.08) (Table 2).
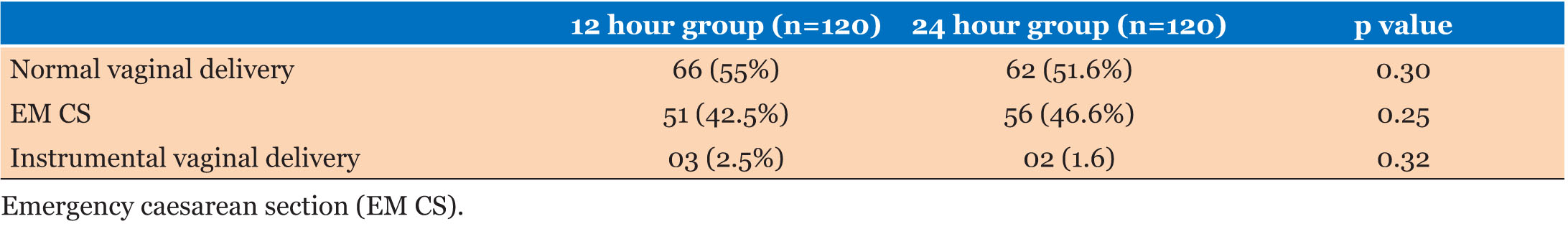
Overall 44.5% (107/240) underwent emergency caesarean section and there was no statistically significant association among the two groups to having an emergency caesarean section. In the 12 hour group caesarean section rate (42.5%) and in 24 hour group caesarean section rate were (46.6%); (p=0.25). More emergency caesarean sections were performed for lack of progress in labor in both groups.
Vaginal delivery and instrumental vaginal deliveries are comparable in both groups. Overall 53.3% delivered vaginally. Sixty six women (55%) out of 120 in the 12 hour group delivered vaginally, whereas 62 women (51.6%) out of 120 in the 24 hour group delivered vaginally; (p=0.30). In the 12 hour group instrumental delivery rate was 2.5% (03/120) and in the 24 hour group it was 1.6% (02/120); (p=0.32) (Table 3).
Considering the adverse outcomes observed during the intrapartum period there was no difference in uterine hyperstimulation, non-reassuring fetal cardiac status by cardiotocography and meconium stained amniotic fluids in both the 12 hour group as well as 24 hour group. In the 12 hour group uterine hyperstimulation was observed in 6.6%, non-reassuring cardiac status was observed in 17.5% and meconium stained amniotic fluid was seen in 14.1% of the women studied. In the 24 hour group uterine hyperstimulation, non-reassuring fetal cardiac status and meconium stained amniotic fluids was observed in 5% (p=0.29), 14.1% (p=0.24), and 17.5% (p=0.24), respectively (Table 4).
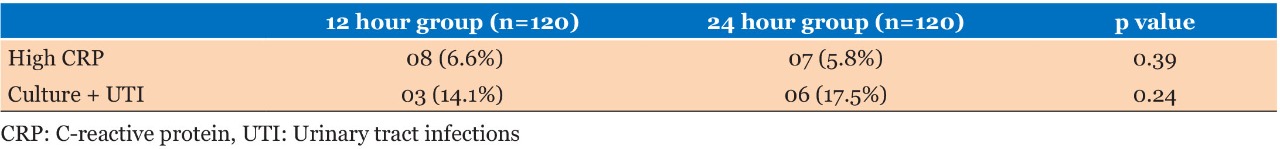
There were no differences in observed neonatal outcomes in the two groups. The Apgar score at 5 minutes, rate of special care baby unit admission, neonatal sepsis, surfactant deficient lung disease, congenital pneumonia, meningitis, necrotizing enterocolitis, neonatal hypoglycemia, neonatal jaundice, and meconium aspiration syndrome was comparable in both groups (Table 5). Considering the maternal morbidity in the 12 hour group, there was one woman with blood culture positive sepsis, and 6.6% (8/120) had elevated C-reactive protein, whereas in the 24 hour group 7 (5.8%) women had elevated levels of C-reactive protein. There were significantly more culture positive urinary tract infections seen in the 24 hour group [5% (6/120)] compared to the 12 hour group (0.8%, 1/120); (p=0.0274) (Table 6).
Discussion
To our knowledge, this is the first randomized controlled trial to compare the effectiveness, acceptability and possible side effects of keeping a transcervical foley catheter for 12 hours versus 24 hours as a method of cervical ripening in a primiparous woman with prolonged pregnancy.
According to our study there were no major differences in effectiveness, acceptability and maternal and fetal side effects in the compared groups, except that culture positive urinary tract infections were common among the 24 hour induction group.
The change in Bishop’s score over 12 hours and 24 hours was comparable in both groups. This was the observed primary outcome of the study. Induction to delivery time is also comparable in the 12 hour group and the 24 hour group.
There were no significant differences in intrapartum maternal complications such as uterine hyperstimulation and chorioamnionitis in both groups neither was a significant difference seen in major fetal complications such as neonatal intensive care admissions and neonatal sepsis. There was no significant difference in pain scores among the 12 hour group and the 24 hour group after 12 hours and after 24 hours, respectively.
The universally accepted time period to keep foley catheter is 12 hours to 24 hours, because of the possibility of chorioamnionitis and neonatal infections, when keeping foley catheter for more than 24 hours.
A randomized controlled trial by Wickramarathna et al (2016) compared the effectiveness and safety in keeping the intra cervical foley catheter for 24 hours versus 48 hours for induction of labor [20] and there was significant difference in the spontaneous onset of labor when the foley catheter is kept in for 48 hours compared to 24 hours (32.7% vs 57.4%, p=0.001). The maternal infectious morbidity and neonatal outcome showed no significant differences (8.5% vs 8.4%, p=0.23). But this study included primiparous as well as multiparous women without considering the age and the sample size of the study was not sufficient, thus reducing the power of the study.
A randomized trial conducted by Ning Gu et al. (2015) determined the optimal foley catheter balloon volume (30 mL vs 80 mL) and the maximum time for cervical ripening (12 hours vs 24 hours) to improve vaginal delivery rate within 24 hours of induction [21]. According to their study 12 hour foley catheter groups achieved vaginal delivery than 24 hour foley catheter group (30 mL/12 hours: 54.5%, 30 mL/24hours: 33.1%, 80 mL/12 hours: 46.4%, 80 mL/24 hours: 24%, p<0.001). Furthermore, caesarean section rate and the incidence of chorioamnionitis were same in all four groups. But this study also included primiparous and multiparous women for the study. Indications for the induction of labor and the gestation of the induction of labor vary from individual to individual. That study did not record women satisfaction and pain score during the ripening time. In contrast our study assessed the primigravida woman in prolonged pregnancy.
Hence, our study shows that those who are practicing the 24 hour method can still get the same effectiveness of the intra cervical foley catheter by keeping the catheter for 12 hours without a change in the side effect profile. In addition, for those who need pre-induction in a short period of time it can be achieved with the same effectiveness in 12 hours as same as in 24 hours.
Considering the strength of the study, this was a randomized controlled trial. Additionally, we recruited only nulliparous women with age ranges from 20 years to 35 years. This increases the statistical power of the study. The sample size was also more reasonable than the previously mentioned trial, which compared the effectiveness of keeping intra cervical foley catheter for 24 hours versus 48 hours.
Our study was conducted in a main teaching hospital in Gampaha district I, Sri Lanka, and in considering the ethnic characteristics in the Gampaha district as well as the population of draining areas to the hospital; it is more or less similar to the ethnic diversity in Sri Lanka. Therefore, these study results are applicable to the Sri Lankan population. Furthermore, this study was done in a low-cost setting. So, study results can be applicable to institutions with low resource setting.
The potential limitations of our trial are also worth mentioning. First, although we calculated sample size prior to this trial, to ensure adequate power to examine our primary outcome, we may have overlooked the power to detect smaller differences in secondary outcomes of the study such as mode of delivery, maternal and fetal complications and side effects. Second, despite the fact that this study was conducted as a randomized controlled trial, blinding could not be performed among participants as well as caregivers. However, other than the time duration of keeping the foley catheter, management of labor procedure was standardized to each patient. As such it is not expected that the unblinding would have an effect on some of the objectively measured outcomes, such as change in Bishop’s score, length of labor, caesarean section rate, and instrumental vaginal rate. Third, the intention of this trial was to determine the efficacy of pre-induction cervical ripening between two groups of participants, no standardized protocol for oxytocin administration.
Conclusion
According to our study there was no difference in achieving pre-induction cervical ripening by keeping intracervical catheter for 12 hours or 24hours. Furthermore, there were no major differences in effectiveness, acceptability, and maternal and fetal side effects in the compared groups. Culture positive urinary tract infections were commonly seen among the women in the 24-hour induction group. Those who are practicing the 24-hour induction method can still achieve the same effectiveness of the intracervical foley catheter by keeping the catheter in for 12 hours. Additionally, for those who need pre-induction in a short period of time it can be achieved with the same effectiveness in 12 hours as same as in 24 hours. Further studies with adequate power need to be done to evaluate the differences in the secondary outcomes.
REFERENCES
1.
Barfield WD; Committee on Fetus and Newborn. Standard terminology for fetal, infant, and perinatal deaths. Pediatrics 2011;128(1):177–81. [CrossRef]
[Pubmed]

2.
Ingemarsson I, Källén K. Stillbirths and rate of neonatal deaths in 76,761 postterm pregnancies in Sweden, 1982–1991: A register study. Acta Obstet Gynecol Scand 1997;76(7):658–62. [CrossRef]
[Pubmed]

3.
Clausson B, Cnattingius S, Axelsson O. Outcomes of post-term births: The role of fetal growth restriction and malformations. Obstet Gynecol 1999;94(5 Pt 1):758–62. [CrossRef]
[Pubmed]

4.
Divon MY, Haglund B, Nisell H, Otterblad PO, Westgren M. Fetal and neonatal mortality in the postterm pregnancy: The impact of gestational age and fetal growth restriction. Am J Obstet Gynecol 1998;178(4):726–731. [CrossRef]
[Pubmed]

5.
Magann EF, Perry KG Jr, Dockery JR Jr, Bass JD, Chauhan SP, Morrison JC. Cervical ripening before medical induction of labor: A comparison of prostaglandin E2, estradiol, and oxytocin. Am J Obstet Gynecol 1995;172(6):1702–6. [CrossRef]
[Pubmed]

6.
Riskin-Mashiah S, Wilkins I. Cervical ripening. Obstet Gynecol Clin North Am 1999;26(2):243–57. [CrossRef]
[Pubmed]

7.
Bujold E, Blackwell SC, Hendler I, Berman S, Sorokin Y, Gauthier RJ. Modified Bishop’s score and induction of labor in patients with a previous cesarean delivery. Am J Obstet Gynecol 2004;191(5):1644–8. [CrossRef]
[Pubmed]

8.
Siddiqui S, Zuberi NF, Zafar A, Qureshi RN. Increased risk of cervical canal infections with intracervical Foley catheter. J Coll Physicians Surg Pak 2003,13(3):146–9.
[Pubmed]

9.
Ekman G, Forman A, Marsál K, Ulmsten U. Intravaginal versus intracervical application of prostaglandin E2 in viscous gel for cervical priming and induction of labor at term in patients with an unfavorable cervical state. Am J Obstet Gynecol 1983;147(6):657–61. [CrossRef]
[Pubmed]

10.
11.
Al-Sebai MAH, Manasse PR. Induction of labour in primigravid women with an unfavourable cervix: A prospective comparative study of prostaglandin E2 vaginal tablets and gel. Journal of Obstetrics and Gynaecology 1993;13(2):112–3. [CrossRef]

12.
Campbell JM. Induction of labour using prostaglandin E2 pessaries. Clin Exp Obstet Gynecol 1984;11(1–2):1–5.
[Pubmed]

13.
Lin A, Kupferminc M, Dooley SL. A randomized trial of extra-amniotic saline infusion versus laminaria for cervical ripening. Obstet Gynecol 1995;86(4 Pt 1):545–9. [CrossRef]
[Pubmed]

14.
Pennell CE, Henderson JJ, O’Neill MJ, McChlery S, Doherty DA, Dickinson JE. Induction of labour in nulliparous women with an unfavorable cervix: A randomized controlled trial comparing double and single balloon catheters and PGE2 gel. BJOG 2009;116(11):1443–52. [CrossRef]
[Pubmed]

15.
Wijepala J, Najimudeen M. Comparison of 30 ml and 60 ml foley catheter for cervical ripening. European Scientific Journal 2013;9(6). [CrossRef]

16.
Heinemann J, Gillen G, Sanchez-Ramos L, Kaunitz AM. Do mechanical methods of cervical ripening increase infectious morbidity? A systematic review. Am J Obstet Gynecol 2008;199(2):177–8. [CrossRef]
[Pubmed]

17.
Bujold E, Blackwell SC, Hendler I, Berman S, Sorokin Y, Gauthier RJ. Modified Bishop’s score and induction of labor in patients with a previous cesarean delivery. Am J Obstet Gynecol 2004;190(5):1644–8. [CrossRef]
[Pubmed]

18.
Garra G, Singer AJ, Taira BR, et al. Validation of the Wong-Baker FACES pain rating scale in paediatric emergency department patients. Acad Emerg Med 2010;17(1):50–4. [CrossRef]
[Pubmed]

19.
Noordzij M, Tripepi G, Dekker FW, Zoccali C, Tanck MW, Jager KJ. Sample size calculations: Basic principles and common pitfalls. Nephrol Dial Transplant 2010;25(5):1388–93. [CrossRef]
[Pubmed]

20.
Wickramasinghe RPTB, Senanayake H, De Silva C. Intrauterine Foley catheter for 48 versus 24 hours for cervical ripening: A randomized controlled trial. Int J Gynaecol Obstet 2020;149(2):225–30. [CrossRef]
[Pubmed]

21.
Gu N, Ru T, Wang Z, et al. Foley catheter for induction of labor at term: An open-label, randomized controlled trial. PLoS One 2015;10(8):e0136856. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Acknowledgments
I would like to thank patients who participated in this paper for her immense support throughout the study.
Author ContributionsDilan Malinda Casather - Conception of the work, Design of the work, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
RNG Rajapaksha - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2021 Dilan Malinda Casather et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.